Convergent is a product of Leap Orbit LLC | Copyright© 2023
Delegated Roster Management: Best Practices for Payers by Jake Tunney, Business Development Manager, Leap Orbit Provider Network Development and Management Executive, Loretta Haythorn, joined us on Interoperability Roundtable for a conversation on Delegated Roster Management: Best Practices. Below is a recording and written recap of our conversation.
VillageCare used Convergent to Automate Their PNDS Reporting Error Resolution
Compliance with No Surprises Act’s Provider Directory Requirements Using Convergent Provider directory requirements have changed with the introduction of the No Surprises Act; data accuracy has become not just a regulatory requirement but a necessity for maintaining trust and efficiency in healthcare. This webinar reveals how Leap Orbit‘s interoperable provider data platform, Convergent, is revolutionizing…
The Convergent Provider Data Platform reduces the costly burden of maintaining provider data. Convergent is a product of Leap Orbit, the trusted innovation partner to the leading health data networks.
Convergent is a product of Leap Orbit LLC | Copyright© 2023
Enhance your health plan's member experience with our three-step approach, focusing on provider data quality assessment, strategic improvements, and tech-driven solutions.
Discover how to leverage accurate, comprehensive provider data to offer personalized care, aiming to elevate care standards and establish your plan as a leader in member satisfaction. Start by identifying your existing data quality and gaps in member experience delivery. You can then create a strategy to implement tech-driven solutions that enrich provider data for accuracy, completeness, and robustness, ensuring that every member interaction is informed and tailored.
The goal is to not only elevate the standard of care but also position your health plan as a leader in delivering exceptional member experiences. Here's your step-by-step plan:
Whether you’re at the beginning or middle of your initiative to investigate and improve member experience, bring your questions to the team here at Leap Orbit. We love talking shop, and are available as a resource throughout your journey.
Ready to get started? Sign up for a free custom provider data quality assessment with one of our experts.

by Jake Tunney, Product Manager, Leap Orbit

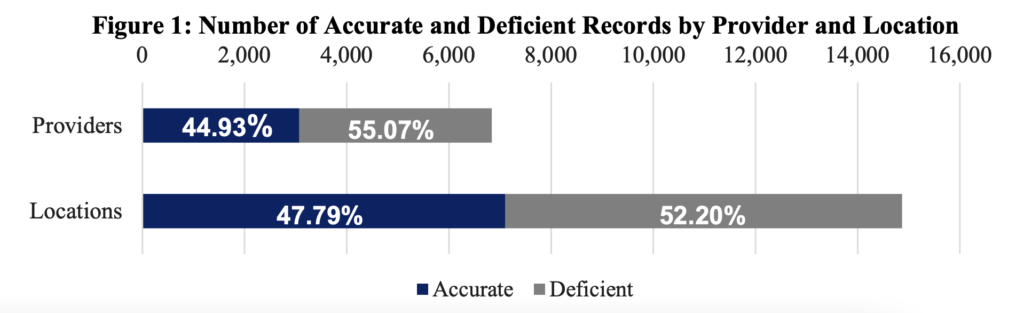
Trust is a firm belief in the truth of something, and trust in provider network data has been notoriously low. A provider network, as a member sees it, is their health insurance’s online directory. What a member doesn’t see is the many data sources and thousands of hours it takes to curate this data. It’s no wonder the trustability for many directories is so low. These lengthy data curation processes are manual, time-consuming, and unfortunately often result in inaccurate, out-of-date information. CMS even found that up to 50% of provider records were inaccurate. Obviously, we can do better here.
Establishing a Benchmark
In order to improve we need to know where we are. One approach is to create a “Data Trust Score.” A Data Trust Score is a single number that distills trust components into one number. The Data Management Association has established a standard of six dimensions that determine data trust. They are:
1. Accuracy - does our data describe the real-world object in question?
2. Completeness - is all our data present that is needed to perform a critical task?
3. Consistency - do our values conflict with each other?
4. Timeliness - is the data available when expected and needed?
5. Uniqueness - is our data free from duplicates?
6. Validity - does it conform to the specific format?
Here’s how we mapped these dimensions to provider data and evaluated the data trust for one of our Health Plan customer's network data:

Their data source originally scored an 84% trust score. That's a solid B. Now that we have our starting benchmark we can track it over time, and look to improve its composite elements.
After implementing Convergent, the customer was able to improve their trust score to 99% - seeing improvements in each dimension after just eight weeks.
Where do we go from here?
Provider data trust doesn't have to be an ambiguous concept. We can set benchmarks and test how well our data performs against them. And if you’re interested, we can get you a complimentary data trust score here.
In part 2 we’ll look at once we have this benchmark, how to use and improve your data trust score.
Implement a framework for selecting a provider data automation partner, focusing on transparency, effective implementation, and user adoption.
The sheer volume of data generated and collected in healthcare today is staggering. From patient records and provider details to billing information and treatment outcomes, the digital footprint of the healthcare industry is vast and continuously expanding. This proliferation of data presents both an opportunity and a challenge.
Managing provider data efficiently is crucial for payers to ensure accurate and up-to-date information is available to members and governing bodies. But every health plan is unique, so how can organizations make an informed decision?
This guide provides a framework for choosing a provider data automation partner, emphasizing transparency, effective implementation, and user adoption.
Transparency is Trust: Start by evaluating if potential partners offer a "glass box" approach rather than a "black box" solution. This means you should fully understand how the data is processed, updated, and maintained.
Questions to Ask:
Case Study Insight: A customer found their provider data often incorrect, impacting consumer and provider trust. The lesson here is the importance of a partner who can offer transparency and accountability in their data processing methods.
Focus on Process: A successful partnership goes beyond just software; it includes a seamless and effective implementation process. Look for a partner with a reliable project management process and the ability to respond and adapt quickly.
Questions to Ask:
Implementation and Customization: Ensure the solution can be customized to fit your unique business processes and operational challenges, thereby enhancing efficiency and productivity.
Achieving Buy-In: Long-term success depends on the solution's adoption across your organization. This involves understanding and aligning with users' needs, offering the necessary tools and resources for them to succeed.
Questions to Ask:
Collaboration and Communication: A partner should work closely with you not just during the implementation but throughout the entire partnership, showing a commitment to your success and adapting to your evolving needs.
While data holds the potential to transform patient care and operational efficiency, managing it through manual processes is not only impractical but also prone to errors, inefficiencies, and delays. Automation is becoming a necessity for plans to maintain adequacy and avoid penalties, and offers an efficient and cost-effective way to harness the power of this data. By transitioning from manual to automated data management processes, healthcare organizations can ensure accuracy, enhance accessibility, and ultimately deliver a better member experience while navigating the complexities of the modern healthcare ecosystem.
Choosing the right provider data automation partner is a critical decision. By focusing on transparency, effective implementation, and long-term adoption, you can select a partner that aligns with your goals and supports the delivery of accurate and reliable provider data. If Convergent is among your options for a provider data management solution, we’d be happy to answer these questions for you!
Contact us today to start the conversation.
by David Finney, Partner & Co-Founder, Leap Orbit

Struggling to navigate the complexities of the CMS Interoperability Rule? You're not alone.
The Centers for Medicare & Medicaid Services (CMS) issued the CMS Interoperability and Prior Authorization Final Rule (Final Rule) on Jan. 17, 2024. The Final Rule focuses on improving prior authorization processes and access to interoperable patient data (by patients, providers, and payers).
The Final Rule applies to:
The May 2020 CMS Interoperability and Patient Access rule established a technological foundation on which the Final Rule was built, requiring payers to implement an HL7® FHIR® Patient Access API. Under the Final Rule, payers are required to add information about prior authorizations (excluding prescription drugs) to the data available via the Patient Access API. It also expands the Merit-based Incentive Payment System (MIPS) to increase the adoption of electronic processes.
No doubt the patient access component is most daunting, with 64% of payers indicating in a readiness survey that this is their biggest concern. Making sensitive patient data available via API is a significant technical challenge, even for many larger organizations. Complexities associated with consent management and privacy and security must be navigated. The risk profile of launching such a service is very high.
With this in mind, it’s understandable that many plans picked a technology vendor with expertise in patient access as their one-stop-shop for a solution to the entire Interoperability Rule. Many of those vendors are offering to throw in a provider directory API solution as a bonus. But there’s peril for plans following this path of least resistance -- and many of them are starting to feel it now. Look no further than other regulatory action, including the federal No Surprises Act, for proof that implementing the provider directory API should be a strategic investment more than an afterthought.
There is a way for your health plan to future-proof your provider data operation, and it's not too late to switch in a painless, cost-effective way. Just like Salesforce and Google have revolutionized other sectors with cloud-native data management platforms, a good provider data management platforms can be deployed and configured in a matter of days, dramatically shortening a customer’s time to value. Choosing such a platform also eliminates much of the execution risk inherent in the implementation of custom enterprise software.
The Convergent Provider Data Hub bridges the gaps in fragmented, poor-quality provider listings across institutions, systems of care, and technology platforms. This data-as-a-service solution uses proprietary matching and cleansing algorithms to sift through and unify provider data from large public and proprietary data sets. The fully FHIR 4.0 compliant suite of APIs and mobile-friendly user interface provide health plans and Medicaid agencies with clean, curated, and always up-to-date network data.
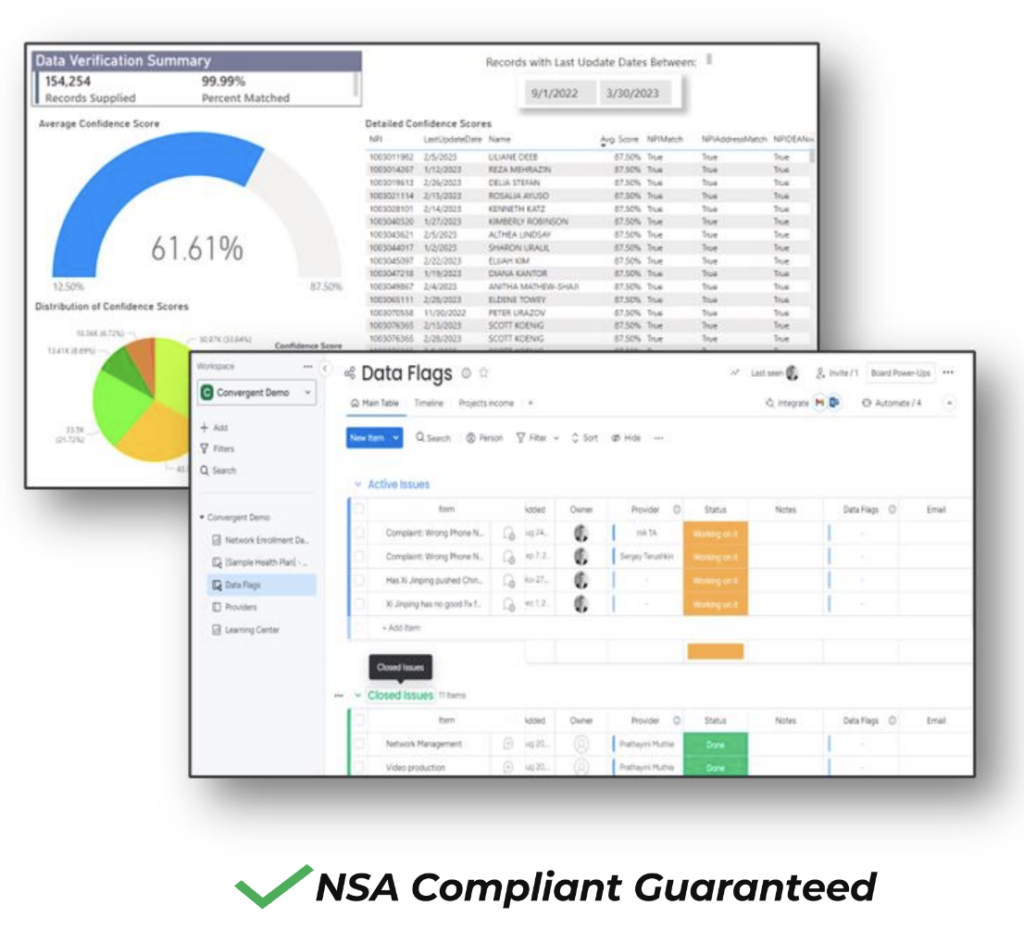
Provider directory requirements have changed with the introduction of the No Surprises Act; data accuracy has become not just a regulatory requirement but a necessity for maintaining trust and efficiency in healthcare. This webinar reveals how Leap Orbit's interoperable provider data platform, Convergent, is revolutionizing compliance and data management in healthcare.
Here are the key sections in this video:
A common challenge in the healthcare industry is that provider data is often inaccurate and time-consuming to maintain, which can cause numerous problems, especially for beneficiaries.
The Centers for Medicare & Medicaid Services (CMS) is beginning to scrutinize this issue more closely and is implementing regulations to address it. Our focus today is on the No Surprises Act, particularly the requirements around validating provider data and ensuring all provider databases and directories are updated within two business days after receiving new information from a provider.
What is Convergent?
Convergent represents the next generation of provider data hubs. Once information is uploaded to Convergent and undergoes standardization, deduplication, and enrichment, this cleansed data becomes instantly available. It can be integrated into your FHIR 4.0 API, member search, or even your claims and clinical systems. We establish continuous feeds that produce what we call a single source of truth, which is then served up into our various API export tools.
ROI of Convergent
The No Surprises Act necessitates a degree of automation and data integration for compliance. This shift can significantly improve longstanding business issues within the industry by automating manual processes that typically take weeks and enhancing data accuracy.
This cuts the two-day turnaround required by the No Surprises Act in half. And instead of the 90-day requirement to verify and update your directory, we're doing this on a continuous basis; validating networks against our nationwide reference set and improving accuracy by up to 90%.
As a result, this gives workforces more time to focus on differentiated tasks instead of manual, repetitive tasks like updating directory data.
With clean data in Convergent, we support multiple integration techniques, including FHIR 4.0 bulk export and CSV export, to utilize this information effectively. Our API-first design ensures compliance with the No Surprises Act by enabling daily data updates.
We can integrate with any modern or legacy provider data system, and we typically like to do this using RPA, or robotic process automation. RPA is source system agnostic and we set these jobs up to run on a continuous basis.
Data Standardization
Once we've grabbed the data, we're putting it in standard format from the major standards bodies like SNOMED and HL7, and even using USPS for address standardization. This improves matching algorithms and deduplication efforts.
Data Deduplication
Upon entering Convergent, we de-duplicate the data using various matching algorithms, such as fuzzy matching and nickname matching. Throughout this data cleansing process, we retain all source records for data provenance, allowing you to search and find all your records that have been merged into the golden record.
Data Validation
Convergent utilizes a nationwide reference set compiled from hundreds of different public and proprietary sources. This data is then mastered within Convergent, including CMS NPPES, OIG SAM sanction bodies, network files, licensure boards, and proprietary sources, among others. We also offer this as a standalone product via API for various applications, such as validating your network or enriching your data.
Data Enrichment
Once we have all that good clean data, we want to be able to use it. We have a number of different integration techniques that we support: FHIR 4.0 bulk export, CSV export, SQL query, provider search, and we integrate with any third-party apps.
We offer a white-label, member-facing provider search that leverages this cleansed data, fully compliant with the Medicaid Managed Care Rule and Section 508.
The integrated provider search feature supports several business functions:
Our API-first design is one aspect that helps us beat the No Surprises Act, automatically updating data on a daily basis instead of every two days.
Inaccurate provider data poses significant challenges, from creating inefficiencies to negatively impacting patient care. Jake outlines how the No Surprises Act is propelling CMS to enforce stricter regulations, requiring updated provider databases within two business days of receiving new information.
Leap Orbit's Convergent offers a groundbreaking solution as a next-generation provider data hub. It standardizes, deduplicates, enriches, and instantaneously makes clean data available across various systems like FHIR 4.0 API, member search, or claims and clinical systems. This innovation not only addresses regulatory compliance but also resolves long-standing business issues by automating manual processes and enhancing data accuracy.
At its core, Convergent is engineered as a Software as a Service (SaaS) platform, meticulously designed to enhance the accuracy of healthcare provider data while ensuring seamless flow between systems. This is not just about data management; it's about fostering a new era of interoperability within the healthcare sector. By facilitating a smoother data exchange, Convergent aims to bridge the gaps between disparate systems, thus enhancing the overall efficiency of healthcare delivery.
Convergent's system automates the directory updating process, surpassing the No Surprises Act's two-day turnaround mandate. Continuous validation against a nationwide reference set ensures up-to-date directories, far exceeding the 90-day verification standard.
The platform's layered solution architecture allows for each layer of the solution to be integrated into existing legacy systems individually, to address specific use cases, or collectively, as a comprehensive platform. This flexibility helps meet the diverse needs of healthcare organizations, regardless of their current tech infrastructure.
Convergent functions downstream of any provider data management system to create a 'golden record' of provider data. Integrating with both modern and legacy systems through robotic process automation (RPA), it operates independent of source systems, validating data continuously.
By adhering to standards set by SNOMED, HL7, and USPS for address standardization, Convergent enhances its matching algorithms, ensuring the deduplication process is thorough yet retains source data for provenance.
Leveraging a comprehensive set of public and proprietary reference sources, Convergent masters the incoming data to create an unmatched validation set. This set can be accessed via API to validate networks or enrich data within Convergent.
Convergent supports multiple integration techniques, maintaining compliance with the No Surprises Act by refreshing data daily. It also features a white-label provider search tool that is 508 compliant, aligning with the Medicaid Managed Care Rule, thus eliminating data silos and fragmented business processes.
As we embrace the demands of the No Surprises Act, technology platforms like Leap Orbit's Convergent become instrumental in maintaining provider directory requirements. With Maryland's Department of Health, CRISP, MedChi, and other institutions already benefiting from Convergent, Leap Orbit invites those interested to explore the potential of their platform for provider data management.
You can try Convergent with a FREE 14-day trial
Ghost networks: they're the healthcare industry's worst-kept secret, lurking in the shadows of provider directories and leaving patients and professionals grappling with the specter of care that's simply not there.
In the labyrinth of healthcare terminology, "ghost networks" may not be a familiar term to everyone. Yet, its significance cannot be understated as it increasingly captures the attention of those within the healthcare sector and the legislative arena. This piece aims to demystify this concept, bringing to light its implications and the buzz it's generating.
Ghost networks refer to the phenomenon where healthcare provider directories in health plans feature professionals who are, in reality, unavailable to offer care. These could be professionals who are no longer practicing, are not taking new patients, or are otherwise erroneously listed as part of a network. On average, data in provider directory entries have over 50% inaccuracy rate, with reports as high as 81% inaccuracy in five of the largest plans. The inclusion of such non-existent providers can have detrimental effects on the service quality of health plans, impacting practitioners, patients, and financial outcomes.
The manifestation of ghost networks can be traced to:
Ghost networks emerge from a complex interplay of factors:
Having providers on your roster that are not actually available to provide care poses several risks:
The surge in concern over ghost networks’ impact on mental health care access has spurred action at the federal and state level:
Tackling ghost networks is crucial for improving the integrity of healthcare provider directories, which in turn enhances patient care, reduces financial wastage, and restores trust in healthcare systems. To curb the prevalence of ghost networks, several strategies are paramount:
By embracing advanced analytics and comprehensive data management strategies, we can eradicate the shadows cast by ghost networks, ensuring a brighter future for healthcare providers, payers, and, most importantly, patients. A survey revealed that 95% of payers plan to prioritize provider data automation tools by 2025.
Learn how to improve your member experience with automated provider data management.
by Jake Tunney, Product Manager, Leap Orbit

I had a call the other day and was dumbfounded: An insurance company I’m sure you know had just bought a provider network management system that will take 3 years to implement.
I get it - healthcare is slow to adapt to new technology. What concerns me is that in this modern era of “automation everything,” healthcare is still solving legacy problems within an legacy paradigm:
“A new system that does a better job than my previous one will improve our results.”
The reality is, that replacing legacy systems with the new legacy systems of the future will not solve provider data problems.
We need a new paradigm to move from task-based workflows to one that leverages modern automation tools like RPA, machine learning, and matching algorithms.
WORKFLOW vs. AUTOMATION
Modern health plan networks are not created in a single provider data management or “PDM” system. They are combinations of delegated rosters, delegated networks, and then direct contracts (plus all of the data sources that go into credentialing these providers).
That results in over 80% of provider data being managed outside of the plan’s PDM. A workflow-based PDM is not designed to handle these disparate sources. An automation-based PDM can ingest data on a continuous basis, algorithmically master, deduplicate, and even enrich that data, and then enable workflows for managing variances when they occur.
If you’d like to see how Convergent enables this new automation-first paradigm for our customers, please click here.
by Jake Tunney, Business Development Manager, Leap Orbit
Many carriers have legacy systems and processes that manage their provider data. The result is a confusing array of manual and semi-automated processes to try to get accurate data to members. When these fail, which they often do, it creates pain for all stakeholders:
However, some carriers are taking an innovative approach to consolidate their provider data operations without upending their old processes and spurring a mutiny among staff members. Here are three reasons why plans need a single source of trust for provider data.
Below is an example of a health plan’s system architecture that leverages this type of architecture. If you’re considering moving to this type of modern infrastructure, contact us here.

5 Ways to Start Improving Provider Directory Trust
by Jake Tunney, Product Manager, Leap Orbit

For the health insurer, when dealing with hundreds of thousands of records from dozens of provider data sources - where do you start? If the goal is to create a directory “Source of Truth,” we can take the following steps:
You can keep doing your provider data entry tasks manually, try to build a system yourself that does this, or you can partner with provider data experts to help move the ball forward. If you’re interested, sign up for a free provider data assessment and trust score calculation.
Ghost providers: they're the healthcare industry's worst-kept secret, lurking in the shadows of provider directories and leaving patients and professionals grappling with the specter of care that's simply not there.
Industry: Health Insurance
Size: Over 1 million members
Plans Offered: HMO, PPO, POS, Medicare and Medicaid
Goal: To promote community health and well-being by ensuring comprehensive coverage and accurate provider information.
Our client faced a significant obstacle with their provider data integrity. The attestation results from its attestation vendor were not meeting the desired standards, with a coverage and accuracy rate lingering around 40%. This data integrity issue posed a risk to the reliability of their healthcare network, member satisfaction, and regulators.
In a decisive move to rectify these shortcomings, the payer partnered with Convergent. The mission was to auto-cleanse and enrich the provider data that was not covered through the standard attestation process. Convergent’s technology and call center was leveraged to sift through data, verify provider details, and update records with accurate, active locations. For those providers that needed additional verification and enrichment, the call center used Convergent to prioritize the highest risk providers for outreach.
The collaboration with Convergent bore significant fruit:
Through this partnership, our client significantly enhanced the reliability of its healthcare network, benefiting over a million members. The case exemplifies how embracing innovative data solutions can overcome complex challenges and drive better health outcomes in the community.
Learn how to improve your member experience with automated provider data management.
by Jake Tunney, Product Manager, Leap Orbit
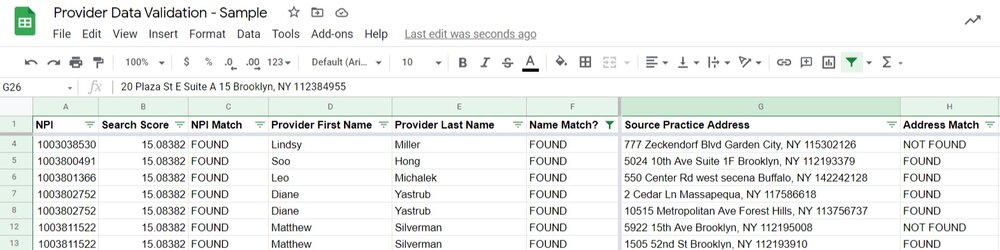
Google Sheets comes with a JavaScript-based language called Apps Script. In this tutorial, we’ll use Apps Script to validate provider NPIs, names, and addresses stored in a Google spreadsheet. This is a quick way to get started using the Convergent provider data validating API, even if you’re not a programmer yourself.
You’ll need a free Convergent API key. If you don’t have one, sign up for an account here. You can do everything in this tutorial with a trial account, though you’ll be restricted to 5,000 validated providers in the first month.
Once you have a Convergent API key, head over to your Google Drive and create a spreadsheet.
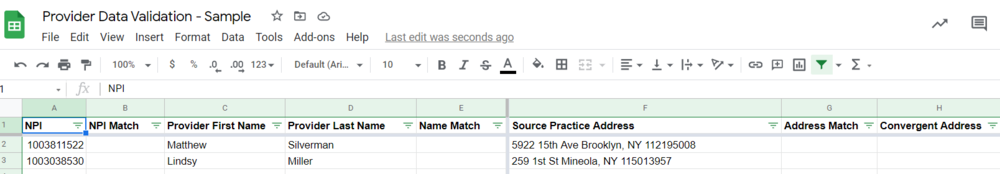
After creating a new Google sheet, create column headings for:
Once you’ve done that, add a couple of rows of provider data. Your sheet should look like this:
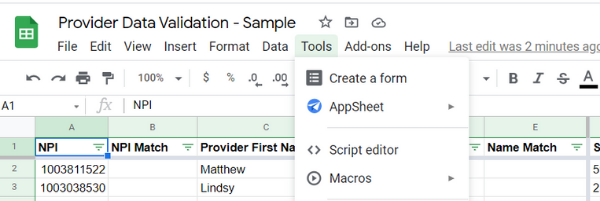
With our data in place, we’re ready to write some code. Click Tools -> Script Editor.
The rest of this post walks you through the code to validate provider data from the spreadsheet. If you’d like to skip to the end and just grab the code, here’s the final product (take note of the placeholders for API Key):
If you want to see how we arrived at that result, we’ll walk you through it in the rest of the post.
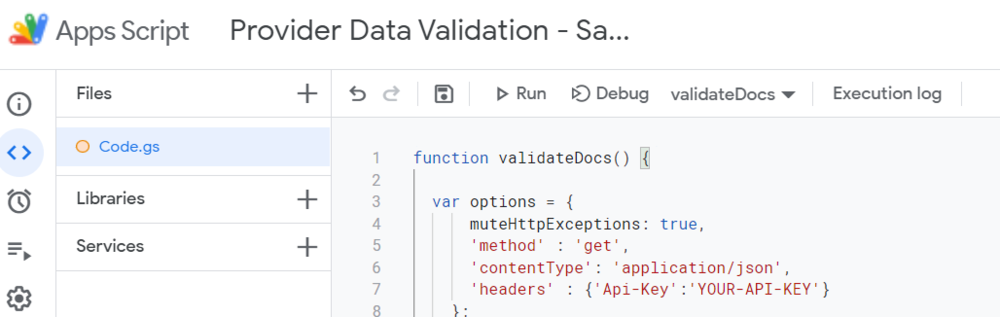
function validateDocs() {
var options = {
muteHttpExceptions: true,
'method' : 'get',
'contentType': 'application/json',
'headers' : {'Api-Key':'YOUR-API-KEY'}
};
var activeSheet = SpreadsheetApp.getActiveSpreadsheet();
var theSheet = activeSheet.getSheetByName("Sheet1");
var NumberofColumns = theSheet.getMaxColumns();
var numRows = theSheet.getLastRow()-1;
var startRow = 2;
var dataRange = theSheet.getRange(startRow,1, numRows, NumberofColumns);
var data = dataRange.getValues();
for (i in data) {
let row = data[i];
let rowNum = parseInt(i) + startRow;
// Convergent NPI Match
let npi = encodeURIComponent(row[0]);
let npiMatch = theSheet.getRange("B" + rowNum);
let url1 = 'https://api.convergent-pd.com/provider/searchSingleBest?NPI=' + npi;
var convergentResponse = UrlFetchApp.fetch(url1, options);
try {
let code = convergentResponse.getResponseCode();
let contentText = convergentResponse.getContentText();
if (code == 404) {
npiMatch.setValue("NO MATCH");
} else if (code == 400 && contentText == "Search returned more than one result.") {
npiMatch.setValue("MORE THAN 1");
} else {
var jsonData = JSON.parse(convergentResponse);
let response = !!jsonData.id;
if (response) {
npiMatch.setValue("MATCH");
//populateConvergentFields(theSheet, rowNum, jsonData);
} else {
npiMatch.setValue("ERROR");
}
}
}
catch (err) {
console.error(err);
return;
}
// Convergent NPI and Name Match
let firstName = encodeURIComponent(row[2]);
let lastName = encodeURIComponent(row[3]);
let npiAndNameMatch = theSheet.getRange("E" + rowNum);
let url2 = 'https://api.convergent-pd.com/provider/searchSingleBest?NPI=' + npi + '&firstname=' + firstName + '&lastname=' + lastName;
var convergentResponse = UrlFetchApp.fetch(url2, options);
try {
let code = convergentResponse.getResponseCode();
let contentText = convergentResponse.getContentText();
if (code == 404) {
npiAndNameMatch.setValue("NO MATCH");
} else if (code == 400 && contentText == "Search returned more than one result.") {
npiAndNameMatch.setValue("MORE THAN 1");
} else {
var jsonData = JSON.parse(convergentResponse);
let response = !!jsonData.id;
if (response) {
npiAndNameMatch.setValue("MATCH");
//populateConvergentFields(theSheet, rowNum, jsonData);
} else {
npiAndNameMatch.setValue("ERROR");
}
}
}
catch (err) {
console.error(err);
return;
}
// Convergent NPI & Address Match
let sourceaddress = encodeURIComponent(row[5]);
let npiAndAddressMatch = theSheet.getRange("G" + rowNum);
let url3 = 'https://api.convergent-pd.com/provider/searchSingleBest?NPI=' + npi + '&address=' + sourceaddress;
var convergentResponse = UrlFetchApp.fetch(url3, options);
try {
let code = convergentResponse.getResponseCode();
let contentText = convergentResponse.getContentText();
if (code == 404) {
npiAndAddressMatch.setValue("NO MATCH");
} else if (code == 400 && contentText == "Search returned more than one result.") {
npiAndAddressMatch.setValue("MORE THAN 1");
} else {
var jsonData = JSON.parse(convergentResponse);
let response = !!jsonData.id;
if (response) {
npiAndAddressMatch.setValue("MATCH");
} else {
npiAndAddressMatch.setValue("ERROR");
}
}
}
catch (err) {
console.error(err);
return;
}
}
}
We’ll write this code in a couple of steps:
First, let’s set up your function with some basics. Add these first lines of code in the app script editor. The “options” variable is what you’ll need to be able to call the Convergent API. Once you’ve registered for your account, add the API key. The second set of variables starting at “activeSheet” grab the data in our spreadsheet that we want to validate.
function validateDocs() {
var options = {
muteHttpExceptions: true,
'method' : 'get',
'contentType': 'application/json',
'headers' : {'Api-Key':'YOUR-API-KEY'}
};
var activeSheet = SpreadsheetApp.getActiveSpreadsheet();
var theSheet = activeSheet.getSheetByName("Sheet1");
var numberofColumns = theSheet.getMaxColumns();
var numRows = theSheet.getLastRow()-1;
var startRow = 2;
var dataRange = theSheet.getRange(startRow,1, numRows, NumberofColumns);
var data = dataRange.getValues();
}
Next, let’s add the for loop we need to traverse the data and apply the queries.
for (i in data) {
let row = data[i];
let rowNum = parseInt(i) + startRow;
}
Let’s validate that our NPIs are actual NPIs. Within the for loop, add the following code. You’ll notice where we ping the Convergent “searchSingleBest” API on the third line, passing the NPIs in the first column. The searchSingleBest endpoint is very similar to our regular search endpoint; however, it uses stricter searching rules and only returns the single best result instead of an array of results. We return “NO MATCH,” “MORE THAN 1,” or “MATCH.”
// Convergent NPI Match
let npi = encodeURIComponent(row[0]);
let npiMatch = theSheet.getRange("B" + rowNum);
let url1 = 'https://api.convergent-pd.com/provider/searchSingleBest?NPI=' + npi;
var convergentResponse = UrlFetchApp.fetch(url1, options);
try {
let code = convergentResponse.getResponseCode();
let contentText = convergentResponse.getContentText();
if (code == 404) {
npiMatch.setValue("NO MATCH");
console.log("[Row: " + rowNum + " NO MATCH]");
} else if (code == 400 && contentText == "Search returned more than one result.") {
npiMatch.setValue("MORE THAN 1");
} else {
var jsonData = JSON.parse(convergentResponse);
let response = !!jsonData.id;
if (response) {
npiMatch.setValue("MATCH");
//populateConvergentFields(theSheet, rowNum, jsonData);
} else {
npiMatch.setValue("ERROR");
}
}
}
catch (err) {
console.error(err);
return;
}
Now we’ll make sure that the doctor’s name tied to the NPI are accurate matches. Paste the following code within the for loop after the above:
// Convergent NPI and Name Match
let firstName = encodeURIComponent(row[2]);
let lastName = encodeURIComponent(row[3]);
let npiAndNameMatch = theSheet.getRange("E" + rowNum);
let url2 = 'https://api.convergent-pd.com/provider/searchSingleBest?NPI=' + npi + '&firstname=' + firstName + '&lastname=' + lastName;
var convergentResponse = UrlFetchApp.fetch(url2, options);
try {
let code = convergentResponse.getResponseCode();
let contentText = convergentResponse.getContentText();
if (code == 404) {
npiAndNameMatch.setValue("NO MATCH");
} else if (code == 400 && contentText == "Search returned more than one result.") {
npiAndNameMatch.setValue("MORE THAN 1");
} else {
var jsonData = JSON.parse(convergentResponse);
let response = !!jsonData.id;
if (response) {
npiAndNameMatch.setValue("MATCH");
//populateConvergentFields(theSheet, rowNum, jsonData);
} else {
npiAndNameMatch.setValue("ERROR");
}
}
}
catch (err) {
console.error(err);
return;
}
Finally, let’s validate our addresses. Addresses are always a bit tricky with docs as they move around and add/remove locations quite a bit. Luckily, Convergent is scouring 100s of public and private sources of data to determine the most accurate, up-to-date addresses. This API query returns a MATCH if we have the source address within Convergent associated with the NPI. A future tutorial will go over how to return our addresses if the source address is invalid. We’re standardizing addresses on the way in so don’t worry if your address data is a tad messy.
// Convergent NPI & Address Match
let sourceaddress = encodeURIComponent(row[5]);
let npiAndAddressMatch = theSheet.getRange("G" + rowNum);
let url3 = 'https://api.convergent-pd.com/provider/searchSingleBest?NPI=' + npi + '&address=' + sourceaddress;
var convergentResponse = UrlFetchApp.fetch(url3, options);
try {
let code = convergentResponse.getResponseCode();
let contentText = convergentResponse.getContentText();
if (code == 404) {
npiAndAddressMatch.setValue("NO MATCH");
} else if (code == 400 && contentText == "Search returned more than one result.") {
npiAndAddressMatch.setValue("MORE THAN 1");
} else {
var jsonData = JSON.parse(convergentResponse);
let response = !!jsonData.id;
if (response) {
npiAndAddressMatch.setValue("MATCH");
} else {
npiAndAddressMatch.setValue("ERROR");
}
}
}
catch (err) {
console.error(err);
return;
}
Now that we have all the code set up, make sure “validateDocs” function is selected, then click “Run.”
This will print out the Convergent responses in the spreadsheet like below:
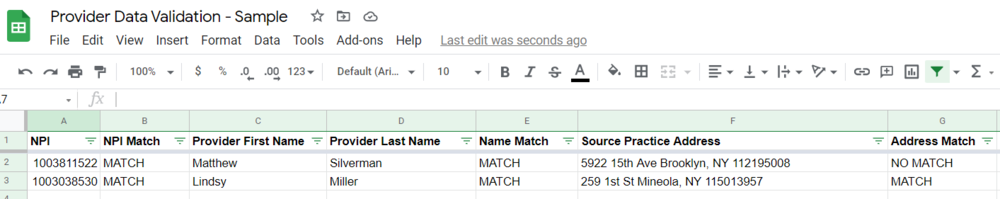
These example providers show how we have valid data across the board except for Dr. Matthew Silverman’s practice address. If we want to go ahead and get his Convergent address, we can parse the JSON response and return that data in the adjacent column(s). We’ll go over how to do that in subsequent tutorials.
If you’d like to get started with the Convergent API, go ahead and grab your credentials here.
by Jake Tunney, Business Development Manager, Leap Orbit

Within the last 2-3 years there’s been a big–and escalating–effort by the federal government to improve both the quality and interoperability of carrier provider data. The intended results include better access to care and the elimination of surprise medical bills. While state health insurance exchanges are not directly subject to the No Surprises Act, the CMS Interoperability Rule, or other new federal policies, there is much to learn and benefit from to offer better service to consumers.
The recent scrutiny from CMS and other regulators has forced carriers to invest in automation and improved data verification efforts. Exchanges can benefit from their improvements and lessons learned. The good news is modern provider data hubs like Convergent have been designed to make the aforementioned processes seamless. Convergent automatically takes messy or out-of-date data from any source and turns it into a highly accurate single source of trust. That way, exchange consumers aren’t getting hampered by bad data and have a better experience with your exchange.
by Jake Tunney, Business Development Manager, Leap Orbit
On October 5th, CMS published an RFI for a National Directory of Healthcare Providers and Services or “NDH.” The NDH would create a “centralized data hub” to once-and-for-all solve the problem of inaccurate provider directories. We applaud CMS’s intention to tackle this perennial, thorny challenge and welcome the chance to provide feedback given our deep experience working with payers, state Medicaid agencies, state-run benefits exchanges, and HIEs in this domain.
Leap Orbit is a healthcare interoperability-focused enterprise technology company founded in 2015. Our vision is to build best-in-class solutions for the healthcare market, using the most modern tools, cutting edge platforms, and modular components under a single umbrella. Since our founding, Leap Orbit has lived up to this vision. Our first major product, a prescription drug motioning platform, is live in Maryland, Nebraska, and Utah, and is being implemented in New Brunswick, Canada.
Our provider directory tool, the Convergent Provider Data Hub, is Leap Orbit’s fastest growing business component. After significant multi-year research and development, we launched Convergent in 2020. Since the launch, our customers in government and the private sector have employed Convergent to rethink the way healthcare provider data is managed and exchanged. We help them navigate the rapidly changing regulatory environment, where accurate provider data is quickly becoming critical infrastructure. We are investing significant resources to expand features to the industry’s premier provider data management platform-as-a-service . We currently cover over 6.1 mm providers with hundreds of different provider types.
Convergent supports the following use cases:
In many ways, the architecture of Convergent reflects the vision that CMS has begun to articulate for the NDH, albeit at the enterprise (and not federal agency) level. Even should a successful NDH be rolled out over time, we do not expect it to alleviate the need for healthcare organizations to maintain their own, interoperable provider data management systems like Convergent. What we envision is a more seamless, well-connected set of provider data sources that rely on key sources of truth, like the NDH, to present accurate and up-to-date provider information where and when it’s needed. We hope that CMS finds our perspective valuable and look forward to continued dialogue on this important topic.
The RFI rightly points out some fundamental problems with current efforts surrounding provider directories:
Although these are all significant problems, we view the first item—inefficient, redundant reporting from providers—as the primary problem, and items two through five are symptoms of that problem. Case in point: on average, provider practices have 20 health plan contracts that require regular status and demographic updates.[1] Each of these has different standards for reporting updates. Many providers have expressed a desire for health plans to align on fewer update channels.[2]
We think addressing this problem is the biggest opportunity presented by this RFI. Resolving redundant reporting channels would be a significant challenge but a massive win for the healthcare industry. But in many key ways, CMS is uniquely positioned to drive the solution. Through tools such as the Quality Payment Program and its authority to regulate state Medicaid programs, Medicare Advantage and other key aspects of the industry, CMS has at its disposal the “carrots and sticks” necessary to bring major change. If CMS is successful, progress on the other use cases identified in the RFP can more easily follow. By solving this central problem, CMS would also establish its credibility in the provider data domain, whereas if it attempts to tackle too many challenges or use cases at once and fails this credibility will be damaged—e.g. CMS will be seen as a part of the problem and not bringing solutions.
For this reason, we strongly suggest CMS take a phased approach, beginning with provider reporting to payers and others and proceeding incrementally by building on demonstrable success. As one example, given our work with HIEs and other customers on interoperability initiatives, we appreciate CMS’s interest in improving access to providers’ digital endpoints, supporting record location for digital exchange, and driving adoption of the Trusted Exchange Framework and Common Agreement (TEFCA). However, we see the complexity of this area and interdependencies with so many other agencies and stakeholders making it a risky set of use cases to pursue at the same time as the one we have recommended above. This is not to say the NDH couldn’t have a role to play; rather, we would advise addressing this area down the road as CMS builds on prior foundational successes.
Below are responses to the questions we believe our experience qualifies us best to respond to.
What benefits and challenges might arise while integrating data from CMS systems (such as NPPES, PECOS, and Medicare Care Compare) into an NDH? What data elements from each of these systems would be important to include in an NDH versus only being available directly from the system in question?
One challenge will always be merging data from disparate data sources and resolving duplicates. Where data sets have NPI that will be less of a problem. However, there are other datasets like state boards that do not have an NPI.
Another challenge is determining which data elements from which source to prioritize over another. For example, do we take specialty from Medicare Care Compare, or from NPPES. Please see "Attachment: CMS & NPPES Data Mapping" for detail on which fields are relevant within the NDH.
An obvious benefit is the convenience of accessing one API to pull all relevant data.
Are there other CMS, HHS (for example, HPMS, Title X family planning clinic locator, ACL's Eldercare Resource Locator, SAMHSA's Behavioral Health Resource Locator, HRSA's National Practitioner Data Bank, or HRSA's Get Health Care), or federal systems with which an NDH could or should interface to exchange directory data?
The core data sets mentioned above are an obvious fit. As datasets expand there need to be explicit use cases that require them. Our view is that the datasets above would initially be consumers of the NDH source of truth data for core provider data attributes. Long-term, NDH may look to add additional, differentiated attributes from these sources.
Are there systems at the state or local level that would be beneficial for an NDH to interact with, such as those for licensing, credentialing, Medicaid provider enrollment, emergency response (for example, the Patient Unified Lookup System for Emergencies (PULSE) [73] ) or public health?
Yes, these all could be relevant depending on the use cases of the NDH. However, if the NDH's initial use case is to resolve redundant provider reporting, we recommend not starting with the state or local level data sets. The core data elements required to facilitate demographic updates and the number of reporting channels are included in "Attachment: Core NDH Fields."
What types of data should be publicly accessible from an NDH (either from a consumer-facing CMS website or via an API) and what types of data would be helpful for CMS to collect for only internal use (such as for program integrity purposes or for provider privacy)?
Also included in "Attachment: Core NDH Fields" in column Public/Private.
We have heard interest in including additional healthcare-related entities and provider types beyond physicians in an NDH-type directory beyond those providers included in current CMS systems or typical payers' directories? For example, should an NDH include allied health professionals, post-acute care providers, dentists, emergency medical services, nurse practitioners, physician assistants, certified nurse midwives, providers of dental, vision, and hearing care, behavioral health providers (psychiatrists, clinical psychologists, licensed professional counselors, licensed clinical social workers, etc.), suppliers, pharmacies, public health entities, community organizations, nursing facilities, suppliers of durable medical equipment or health information networks? We specifically request comment on entities that may not currently be included in CMS systems.
We recommend covering as many provider types as possible. The Medicare FFS Public Provider Enrollment Data Dictionary outlines a set of Provider Type Codes that can be used to enforce conformance around a common set of provider types.
We want an NDH to support health equity goals throughout the healthcare system. What listed entities, data elements, or NDH functionalities would help underserved populations receive healthcare services? What considerations would be relevant to address equity issues during the planning, development, or implementation of an NDH?
There are a number of accessibility features that providers may offer including handicap accessibility, ADA compliance, public transit options, answering service, cognitive support services, and mobility services. Oregon is at the forefront of collecting what is known as "REALD" data which includes race, ethnicity, languages, and disabilities.
What provider or entity data elements would be helpful to include in an NDH for use cases relating to patient access and consumer choice (for example, finding providers or comparing networks)?
What data elements would be useful to include in an NDH to help patients locate providers who meet their specific needs and preferences?
Would it be helpful to include data elements such as provider languages spoken other than English, specific office accessibility features for patients with disabilities and/or limited mobility, accessible examination or medical diagnostic equipment, or a provider's cultural competencies, such as the National Committee for Quality Assurance's Health Equity accreditation (though we note that these data elements may be difficult to verify in some cases)?
Yes
Understanding that individuals often move between public and commercial health insurance coverage, what strategies could CMS pursue to ensure that an NDH is comprehensive both nationwide and market-wide?
CMS, or a federal partner, should examine how to require all plans to publish their directory in a FHIR API; the NDH should then consume that data for plan participation information for each provider.
How should CMS work with states to align federal and state policies to allow all parties to effectively use an NDH?
States are primarily medical license and sanctions issuers. Today there is no unified source of that information. While this data is not necessarily a demographic update, a central repository would be a huge improvement to the current state of affairs. FSMB has already begun this work and could be a viable partner with collecting licensing data on all 50 states.
What types of entities should be encouraged to use data from an NDH? For what purposes and why?
We envision an environment where all providers who receive payment from Medicare are incentivized to keep their information up-to-date in the NDH. Currently, many providers are encouraged to use the ProView tool from CAQH for this purpose (payers are given free access to data feeds from ProView); however, this use is not ubiquitous and CAQH does not possess the same “carrots and sticks” that CMS does to motivate providers to use it.
If this environment became reality, we believe payers would in turn use the NDH as a single source to verify demographic information and practice location information. This would begin to alleviate the major plan of multiple roster submissions and management that all providers and the payers with whom they contract must navigate today. This is a major source of friction and bad outcomes in the provider data domain.
What are some of the functions or features of current provider directories that work particularly well?
What are some of the lessons learned or mistakes to avoid from current provider directories of which we should be aware?
We solicit comments on key considerations related to data submission and maintenance for potential NDH development: What policy or operational factors should be considered for new data collection interfaces as part of a single point of entry?
How can data be collected, updated, verified, and maintained without creating or increasing burden on providers and others who could contribute data to an NDH, especially for under-resourced or understaffed facilities?
CMS can pre-populate provider profiles using the data sources referenced above, and possibly also current claims. These profiles can then contain most of the data points that do not change often, with the ability for the provider to update information that might. We believe if CMS makes it a publicly-stated objective to quickly eliminate the friction providers and payers experience with roster management and tools like ProView, and replace this with a single, national source of truth in the NDH, then stakeholders will be motivated to support its success. Even under-resourced and understaffed organization experience this friction, and consolidating their effort around the NDH could be a meaningful and welcome burden reduction.
What are barriers to updating directory data in current systems that could be addressed with an NDH?
What are current and potential best practices regarding the frequency of directory data updates?
We recommend updating data as soon as a new source update is received. For example, NPPES publishes a weekly update file. The NDH should be able to ingest that information and populate it within the NDH within 24 hours of it being published.
What specific strategies, technical solutions, or policies could CMS implement to facilitate timely and accurate directory data updates?
How could consistent and accurate NDH data submission be incentivized within the healthcare industry?
With regard to providers themselves (both organizations and practitioners), CMS and HHS more broadly have a track record of creatively leveraging incentives to drive the implementation and use of new technologies. We see nothing different about the adoption of NDH. Just as CMS has made Promoting Interoperability requirements a key aspect of MIPS, so too could it incentivize timely, comprehensive reporting to the NDH as a vital part of the provision of quality care. Likewise, ONC should evaluate how to incorporate standards-based reporting to the NDH into future editions of its Standards Version Advancement Process (SVAP) so that relevant technology vendors to the provider community can contribute to enabling solutions.
Likewise, through its authority over state Medicaid programs and managed care as well as Medicare Advantage contracts, CMS can push plans to move towards contracts that require provider data management via the NDH instead of ad-hoc roster submission and third-party portals. Over time, all stakeholders would see gained efficiencies across contracting, credentialing, network building and management and IT.
How should duplicate information or conflicting information reported from different sources be resolved to balance the reporting burden versus confidence in data accuracy?
A cloud-based MDM platform like Convergent uses a matching algorithm to determine which providers are the same across different data sets. We apply a litany of strategies that result in a 99.9% match rate. The remaining duplicates are identified and resolved at the source. We then apply a series of ranking algorithms for each individual field including frequency, date, and source to determine which value at the field should be the "Golden Record." Our preference is typically to use a data source ranking when we have a trusted primary source.
The Healthcare Directory initiative and FAST both identified validation and verification as important functions of a centralized directory. What data types or data sources are important to verify (for example, provider endpoint information, provider credentialing) versus relying on self-reported information? Are there specific recommendations for verifying specific data elements?
Typically, things like license, board certification, and insurance are verified by primary sources while demographic info and location are self-attested. NCQA's credentialing standards are a useful framework when thinking about verification.
What use cases would benefit from data being verified and what sort of assurances would be necessary for trust and reliance on those data?
The NDH should focus its scope on being the primary source for self-attested data. Other use cases may arise in the future after this is successfully executed.
Self-attested data would require data provenance, indicating the date of the update, and the source of the update. The data source can either be the provider themselves or a delegated authority.
Are there use cases where an NDH could provide data that has already been verified to reduce that burden on payers or other entities and, if so, how could that be achieved?
Because demographic data and location data is self-attested, the NDH could be the single source of these updates.
What concerns might listed entities have about submitting data to an NDH? We solicit comments on provider delegation of authority to submit data on a provider's behalf:
While REALD data could be useful, it might also be used to profile providers in a negative way. Awareness of racial and ethnic data could lead to discrimination.
What challenges, if any, occur in the processes for delegating authority to submit data on behalf of providers or in the processes for submitting directory data on behalf of providers?
A bulk upload from a physician group could be submitted that disagrees with what the provider themselves submit. The NDH needs to have an MDM system that enables a hierarchy of preferred data source rankings. In this case we'd want to rank the provider-submitted data over the group submitted data.
Should CMS consider including role-based access management to submit provider data to an NDH, and, if so, what kind of role-based access management?
Yes. HL7 has clear guidelines on identity and access management.
Are there entities that currently exist that would be helpful to serve as intermediaries for bulk data verification and upload or submission to an NDH? If so, are there existing models that demonstrate how this can be done (for instance, the verifications performed through the Federal Data Services Hub)?
Convergent for medical licenses, DEA #'s, Medicaid IDs, USPS Address standardization, OIG and SAM for sanctions, etc.
ABMS and other certification boards for board certification
How do intermediaries currently perform bulk data verification and upload or submission to provider directories?
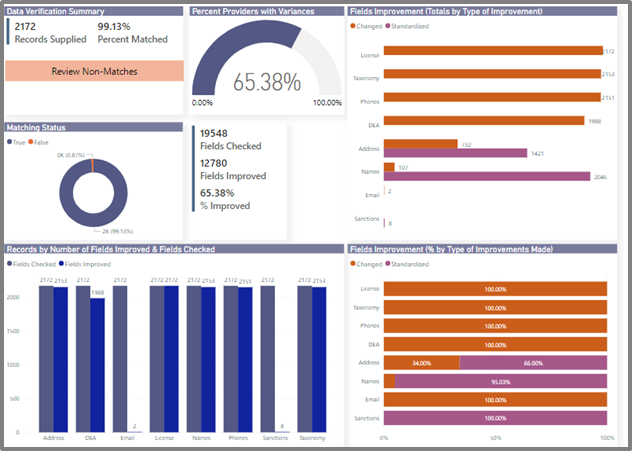
Convergent has a robust process, leveraging our search APIs to bulk query provider records against our nationwide set of reference data. We then auto-generate validation reports based on those results. Below is a sample report.
What functionality would constitute a minimum viable product?
What use cases should be prioritized in a phased development and implementation process for immediate impact and burden reduction?
Single location for provider practice location and demographic updates. It's not even worth considering others until this is accomplished.
What types of entities and data categories should be prioritized in a phased development and implementation process for immediate impact and burden reduction?
All CMS provider types from this file (link) and all data elements under the Convergent-prescribed NDH Core Data Set.
How could human-centered design, including equity-centered design, principles be used to optimize the usability of an NDH?
We would recommend using the Design Sprint methodology established by Google Ventures (http://www.gv.com/sprint/). This provides a user-centric design approach that equally values expert input and end-user feedback.
What are the most promising efforts that exist to date in resolving healthcare directory challenges? How could CMS best incorporate outputs from these efforts into the requirements for an NDH? Which gaps remain that are not being addressed by existing efforts?
How could NDH use within the healthcare industry be incentivized? How could CMS incentivize other organizations, such as payers, health systems, and public health entities to engage with an NDH?
With regard to providers themselves (both organizations and practitioners), CMS and HHS more broadly have a track record of creatively leveraging incentives to drive the implementation and use of new technologies. We see nothing different about the adoption of NDH. Just as CMS has made Promoting Interoperability requirements a key aspect of MIPS, so too could it incentivize timely, comprehensive reporting to the NDH as a vital part of the provision of quality care. Likewise, ONC should evaluate how to incorporate standards-based reporting to the NDH into future editions of its Standards Version Advancement Process (SVAP) so that relevant technology vendors to the provider community can contribute enabling solutions.
Likewise, through its authority over state Medicaid programs and managed care as well as Medicare Advantage contracts, CMS can push plans to move towards contracts that require provider data management via the NDH instead of ad-hoc roster submission and third-party portals. Over time, all stakeholders would see gained efficiencies across contracting, credentialing, network building and management and IT.
[1]https://www.caqh.org/about/newsletter/2019/caqh-white-paper-hidden-cause-inaccurate-provider-directories
[2]https://www.caqh.org/sites/default/files/other/CAQH-AMA_Improving%20Health%20Plan%20Provider%20Directories%20Whitepaper.pdf
How technology can transform healthcare administration, making it more agile, compliant, and focused on providing high-quality member experiences.
VillageCare, a prominent New York-based MLTC, D-SNP, and MA carrier, faced significant hurdles with their manual provider data management process. Their outdated vendor system, reliant on cumbersome spreadsheet uploads, led to stale and inaccurate provider data. Additionally, complying with network adequacy reporting was time-consuming and prone to errors.
Their previous provider directory vendor required uploading a master spreadsheet for updates, taking an average of 45 days for an update. VillageCare's provider data had to be manually transformed from numerous roster templates to map to the master spreadsheet, resulting in stale, inaccurate data for members.
This led to time-consuming and error-prone network adequacy reporting through the Provider Network Data System (PNDS). Key data was missing and they would consistently submit out-of-date information. Insurers that issue commercial non-MCO medical, stand-alone dental, or stand-alone vision products in New York are required submit their networks to the Department of Financial Services for quarterly review through PNDS.
Network adequacy reporting resulted in an error report like the following:

Stuart Meyer, as CIO, has been pivotal in transforming VillageCare into a data-driven organization. This transformation included the technical adoption of cloud-based strategies and significant enhancements in employee data literacy and data governance. Meyer's leadership underscores VillageCare's commitment to leveraging data for strategic decision-making and operational efficiency.
VillageCare's response to stringent regulatory demands, such as the CMS Interoperability Rule and the No Surprises Act, was to adopt FHIR-based solutions. This move not only ensured compliance but also significantly improved the accuracy and timeliness of their provider data management. The integration of Leap Orbit’s Convergent platform further streamlined the process, reducing the update cycle from 45 days to less than 24 hours, thereby exceeding the two-day update requirement mandated by new regulations.
Enter Convergent, the game-changing provider data management hub from Leap Orbit, to streamline VillageCare's operations. Leap Orbit's data engineering team partnered with Ku'uipo Fales, VillageCare's AVP of Data Management, to seamlessly integrate Convergent within VillageCare's infrastructure. They collaborated on an automation design that shrunk their 45-day directory update process to under 24 hours, well below the 2-day update window required by the No Surprises Act.
"Convergent revolutionized our operations by allowing us to shift to an automated, two-day refresh cycle. This change was crucial, as it removed the need for manual interventions, streamlining our entire data management process and ensuring our compliance with timely and accurate network reporting requirements." - Ku'uipo Fales, VillageCare, AVP of Data Management
They also aligned on a set of enrichment strategies that leveraged Convergent's "out-of-the-box" primary source reference data, and added new sources unique to VillageCare's requirements. These sources automatically enriched VillageCare's provider data in a way that eliminated network reporting critical errors and resolved most soft errors. This resulted in a dramatic reduction in manual effort by the plan and an improvement in accuracy. Convergent enrichment data was leveraged in the following ways:
Ku’uipo Curry, Director of Data Management at VillageCare, highlighted the organization's focus on enhancing the member experience through user-friendly, 508-compliant interfaces designed by Leap Orbit. The new systems are praised for their simplicity and effectiveness, making them more accessible, especially to older adults with visual impairments. The improved interface has been so effective that even internal staff prefer using the member search tools over older internal systems.
The automation introduced by Convergent has not only streamlined operations but also significantly reduced manual errors and compliance risks. This transformation has enabled VillageCare to focus more on strategic initiatives rather than operational fire-fighting.
VillageCare achieved an automated provider directory, ensuring No Surprises Act compliance. Their PNDS submission for network adequacy reporting saw critical errors reduced to zero, and soft errors reached an all-time low. Leap Orbit's automation significantly accelerated error resolution, resulting in VillageCare's cleanest and most accurate PNDS files to date.
“For our PNDS submission, Leap Orbit's automation helped resolve the majority of critical errors that usually took days to research various websites, source files, and reference documents, which resulted in our cleanest and most accurate PNDS files to date.” - Melissa Leudeman, VillageCare Network Manager
The integration of FHIR APIs and the automation brought by Convergent are more than just technical upgrades for VillageCare; they represent a strategic realignment towards more efficient, compliant, and member-focused operations. This case study exemplifies how technology can transform healthcare administration, making it more agile, compliant, and focused on providing high-quality member experiences.
Contact us here if you'd like to transform your provider data management with Convergent.
Leap Orbit, the innovation partner to market-leading health data networks, announced today that has been awarded a new contract from the Washington Health Benefit Exchange, Washington’s state-based exchange. Leap Orbit’s Convergent Provider Data Hub will deliver comprehensive, up-to-date provider information to power the Exchange’s online marketplace, Washington Healthplanfinder.
“We are thrilled to be working with the Exchange team to support the one in four Washingtonians who rely on Healthplanfinder to search for, compare and enroll in affordable health and dental insurance,” said David Finney, partner and co-founder of Leap Orbit. “Accurate provider data is at the heart of the shopping experience, and Convergent will help consumers confidence in selecting the network that’s right for them.”
Convergent easily marries imperfect health plan network data files with a proprietary, nationwide set of reference data for clean, up-to-date provider data. By using exclusively modern, cloud-native components and shared reference data, Convergent delivers powerful provider data tools much more affordably than legacy provider data management systems.
In addition to state-based insurance exchanges, Convergent also supports the needs of carriers, government agencies and provider organizations. Beyond the core cloud-based Provider Data Hub, the Convergent platform includes a growing set of modules to support specific business challenges. These include:
Convergent also supports integration with industry-leading, third-party components such as CAQH ProView, DocuSign Contract Lifecycle Management, Monday.com CRM and Microsoft PowerBI.
About Convergent & Leap Orbit
Convergent is the last provider directory investment a healthcare organization will ever make. It seamlessly transforms any source of healthcare provider data into a continuously updated single source of truth. By automating provider data operations for healthcare organizations, Convergent eliminates data silos, improves workforce productivity, and ensures no surprise billing. Simply put, Convergent automatically produces flawless provider directories. Learn more at www.getconvergent.io.
Founded in 2015, Leap Orbit is the trusted innovation partner to market-leading health data networks. Leap Orbit’s philosophy is to run toward healthcare’s biggest challenges, providing technology and solutions to assist with the opioid crisis and patient data privacy. Leap Orbit’s solutions touch the lives of more than 45 million patients from Alaska to Maryland. For more information, visit LeapOrbit.com and follow us on LinkedIn.
About the Washington Health Benefit Exchange
The Washington Health Benefit Exchange was created in state statute in 2011 as a public-private partnership. The Exchange is responsible for the operation of Washington Healthplanfinder, an easily accessible, online marketplace for individuals and families to find, compare and enroll in Qualified Health Plans, Qualified Dental Plans and Washington Apple Health (Medicaid). Washington Healthplanfinder offers Washington state residents:
To learn more about the Exchange, visit www.wahbexchange.org. Open enrollment for Washington Healthplanfinder is from Nov. 1 to Jan. 15, 2023.
by Jake Tunney, Business Development Manager, Leap Orbit
Provider Network Development and Management Executive, Loretta Haythorn, joined us on Interoperability Roundtable for a conversation on Delegated Roster Management: Best Practices. Below is a recording and written recap of our conversation.
by David Finney, Partner, Leap Orbit

At the typical health plan we talk to, provider data touches virtually every business unit. It’s daunting to contemplate a project that involves asking the entire organization to replace systems or change what they do.
Many health plans understand it’s ultimately what’s needed, for regulatory compliance reasons, to free up important human capital, and to improve provider and member relations. Getting there’s the problem.
To alleviate these fears, and to reduce implementation risks, we’ve encouraged plans to embrace what we call “strategic incrementalism.” Consider this a particular brand of change management. (It isn’t an original concept—thanks to our friends and colleagues David Horrocks and Scott Afzal for introducing it to us and showing, consistently over a long period of time, how well it can work.)
Strategic incrementalism starts with a vision of the long-term objective. Then it calls for picking an initial, high-value use case and putting a manageable win on the board. Then do this again ... and again. Over time, organizations build momentum towards the objective, and taking the next step towards it gets successively a little easier each time.

In each case, these are use cases with demonstrable value, institutional backing, and budget approval for the incremental project. They also lay the groundwork for future progress towards the ultimate goal.
These projects involve deploying a modular solution—our FHIRsearch tool, our provider data governance solution, or reporting respectively—while also bringing to bear the Convergent Provider Data Hub, which is the backbone that makes modularity and strategic incrementalism possible. By beginning to load local sources of provider data, cleaning and deduplicate them, and leveraging the power of our national reference data, the table is set to onboard new functional modules after the first demonstration of success.
With the groundwork laid, it gets a little easier each time to tackle a new module. New stakeholder groups within the organization come on board. The plan takes a step closer towards the long-term goal of a single, trusted source of truth for provider data across the enterprise.
Drilling down to the core of Medicaid health plans, the accuracy of provider directories plays a crucial role in ensuring that patients can find and access the care they need. However, maintaining accurate and up-to-date provider information poses significant challenges, exacerbated by data silos, varying roster formats, and differing regulations at both federal and state levels. In the face of all of these challenges, a universal standardized roster is something that many states and healthcare organizations consider a pipe dream.
Under the leadership of Samantha Olds Frey, the Illinois Association of Medicaid Health Plans (IAMHP) was successful in creating a universal standardized roster for all Illinois Medicaid managed care organizations (MCOs). Leap Orbit's Convergent entered as a data partner, bolting on automation capabilities following the roster's implementation. In this case study, we've summarized some of the key takeaways from their collaborative, multi-stakeholder approach in achieving healthcare interoperability.
The Medicaid health plans in Illinois faced a multifaceted problem. Lawsuits related to ADA information accuracy in provider directories highlighted significant gaps in the existing processes. At the same time, new CMS regulations and changes in Illinois state law, prior to the No Surprises Act, required health plans to make substantial improvements to their provider directories. These challenges underscored the need for a systematic approach to enhance the accuracy and reliability of provider information.
In Illinois, the need for accurate provider directories became particularly pressing due to lawsuits challenging the accuracy of Americans with Disabilities Act (ADA) information, the first iteration of Centers for Medicare & Medicaid Services (CMS) Mega Rule, and changes in Illinois state law affecting Medicaid provider directories.
The overarching goal was to improve the quality of Medicaid provider directories through a series of targeted objectives:
The journey to a universal standardized provider roster began with a clear recognition of the existing challenges and the need for a cohesive strategy. Health plans decided to collaborate on creating a standardized roster rather than making isolated changes. This involved extensive meetings, discussions, and the joint analysis of existing rosters. Key focus areas included ADA compliance, the adoption of military time for consistency, and the introduction of color coding to simplify data entry.
The process is not for the faint of heart. I had several six- to eight-hour meetings where we were just going through data spreadsheet by spreadsheet, and white-boarding.
Samantha Olds Frey, CEO, IAMHP
Implementing the standardized roster required a comprehensive and coordinated effort. Existing rosters were collected and meticulously analyzed, leading to the standardization of data fields and the addition of crucial ADA information previously overlooked. This phase marked the practical application of Convergent’s capabilities to realize the standardized provider roster:
Feedback was sought from the Department of Healthcare and Family Services, hospital associations, and a select group of hospitals, culminating in a refined roster that received broad acceptance from the provider community. Supportive public policy and legislation further bolstered the adoption process.
After IAMHP created the universal roster, Leap Orbit's Convergent was added to elevate the process with its robust automation services. A key feature introduced by Convergent was automated data validation. This scheduled process meticulously checks for errors or suspicious data entries and promptly sends alerts if any discrepancies are found. Automated data validation ensures that data is error-free and ready for use by verifying its accuracy, completeness, and conformity to predefined standards. This process significantly reduces the need for manual reviews and mitigates the risk of human error. Convergent's validation tools cross-reference data against multiple sources, ensuring a high degree of accuracy and reliability.
Looking to the future, Convergent plans to implement further automation services, including automated data transformation to ensure data is in the required format, automated data submission for seamless integration into various systems, and automated data enrichment/verification to enhance the quality and completeness of the data. These advancements will continue to streamline processes, improve data integrity, and support the ongoing efforts to maintain accurate and reliable provider directories.
The journey towards establishing a universal standardized provider roster in Illinois involved a collaborative effort among various stakeholders. It began with internal discussions within the health plans to identify the need for a common, standardized roster. Subsequently, the plans collected and analyzed existing rosters to identify common fields and streamline the process.
A critical step in the process was engaging external stakeholders, such as hospitals and physician practices, to gain valuable insights and ensure their needs were met. This multi-stakeholder approach allowed for effective communication and problem-solving, even though it involved challenging discussions. Including large healthcare systems and atypical providers early in the process proved beneficial in fine-tuning the roster and making it more comprehensive.
Throughout the process, it became evident that the roster required continuous refinement. Stakeholders held several meetings, discussed various aspects, and made iterative changes to the roster and its instructions. By incorporating feedback and refining the roster through testing and further discussions, a robust and user-friendly solution emerged.
We collected every plan's existing roster at the time. We then went through every field and identified what we wanted to retain and why we thought it was needed. As we worked with stakeholders, some were won and some were lost.
Samantha Olds Frey, CEO, IAMHP
The roster's continued evolution was expected, with periodic updates and improvements to align with changing provider data needs. As provider data quality improves and becomes more accurate, certain fields on the roster might become optional or redundant, leading to a leaner and more efficient solution.
Legislation played a significant role in promoting the adoption of the standardized roster. However, the success of the policy was dependent on the groundwork laid by collaborative discussions and stakeholder buy-in. The legislation mandated all Illinois providers participating with the MCOs use the roster, ensuring nearly 100% participation.
The introduction of the standardized provider roster marked a significant milestone in improving Medicaid health plans in Illinois, including data quality, claims processing, and provider directories. Providers benefited from the standardization, as they no longer needed to fill out multiple, disparate rosters for different health plans. The roster provided a single, streamlined format, simplifying the process and reducing administrative burdens.
We finalized the version and put it out into the world, and then slowly found adoption from the provider community.
Samantha Olds Frey, CEO, IAMHP
Notable outcomes included:
The success story of the universal standardized roster in Illinois demonstrates the power of a collaborative, multi-stakeholder approach in achieving healthcare interoperability. By fostering open dialogue, addressing challenges, and embracing feedback, the implementation process became more efficient and effective. As other states consider similar initiatives, Illinois' experience serves as a valuable blueprint for driving positive change in the healthcare industry.
The IAMHP Roster Roster Validation Tool is live. Watch the demo now.
By David Finney
In a season of anxiety, it might be easy to overlook the rising worry about approaching deadlines related to the Interoperability and Patient Access Final Rule. But it’s certainly there. A survey released by the eHealth Initiative last month underscored that, distracted by COVID and other priorities, many health plans and Medicaid agencies are fretting about their ability to comply on time.
For example, according to eHI, 78% of payers reported that their ability to get ready for the Interoperability Rule has been hindered in some way by COVID. Most of the industry is probably hoping for further enforcement discretion (e.g. delays) from the federal government. Whether that comes or not, it’s patient access that is most on the plans’ minds.
No doubt the patient access component of the Interoperability Rule is its most daunting. Making sensitive patient data available via API is a significant technical challenge, even for many larger organizations. Complexities associated with consent management and privacy and security must be navigated. The risk profile of launching such a service is high.
It’s understandable, then, that many plans would pick a technology vendor with expertise in patient access as their one-stop-shop for a solution to the entire Interoperability Rule. Many of those vendors are offering to throw in a provider directory API solution as a bonus. But there’s peril for plans following this path of least resistance. Here are three reasons why implementing the provider directory API should be a strategic investment more than an afterthought.
1. Choosing a solution wisely can address perennial challenges such as provider credentialing and network management.
According to CAQH, managing provider data is a $2 billion-per-year exercise—and still often an exercise in futility. Additionally, CMS has the authority to fine health plans up to $25,000 per Medicare beneficiary for deficiencies in Medicare Advantage plan directories and up to $100 per beneficiary for errors in QHPs in the ACA exchanges. Beyond the immediate financial implications, poor provider directories create barriers to care for members, result in lost revenue for plans, and cause delayed and denied claims. Simply adding a thin layer of FHIR compliance to an existing provider dataset is a missed opportunity. A more robust, purpose-built provider directory solution that leverages reference data from a broad range of public and proprietary data sets, along with sophisticated matching and cleansing algorithms, can result in cleaner, curated provider data to inform a plan’s upstream business processes. Reference data allows plans to benefit from the “wisdom of the crowd,” capitalizing on primary-source outreach and data quality improvements to directories made elsewhere instead of constant manual effort.
2. Plans subject to the Medicaid Managed Care 2020 Final Rule must meet additional, more complex provider directory requirements.
The Interoperability Rule and the new MMC Final Rule are designed to be complementary. The Interoperability Rule requires publishing an API (digital endpoint / machine usable) that returns at minimum a pretty limited set of provider attributes, while the MMC Final Rule requires plans to publish an online and mobile-friendly directory (human usable, including by members with disabilities) with a more extensive set of provider attributes. The same underlying provider data model can support both of these requirements, serving up provider data for both the API and the mobile-friendly web interface. Many plans that offer a provider search function on the web today have not optimized it for mobile to the extent CMS is requiring; further, without a detailed understanding of the MMC Final Rule, patient-access vendors may deliver solutions that do not comply with it either. Maryland’s Medicaid program is already utilizing Leap Orbit’s solution, Convergent, to comply with the CMS Interoperability Rule. The provider directory is being deployed in partnership with Leap Orbit’s longtime client CRISP, a regional health information organization that is Maryland’s state designated health information exchange (HIE). CRISP has contracted with MedChi, the Maryland State Medical Society, to provide data stewardship services for the provider directory.
3. Implementing a cutting-edge provider directory solution doesn’t have to be a huge technology project.
Many plans and Medicaid agencies are accustomed to costly, months-long custom software implementations with a waterfall of complex technical and functional requirements. There are many reasons why vendors continue to pitch such projects, not least because they can be highly profitable. But this need not be the case to implement a cutting-edge provider directory. Just as companies like Salesforce and Google have revolutionized other sectors with cloud-native data management platforms, next-generation provider data management platforms like Leap Orbit’s Convergent provider directory can be deployed and configured in a matter of days, dramatically shortening a customer’s time to value. Choosing such a platform also eliminates much of the execution risk inherent in the implementation of custom enterprise software.
Leap Orbit has created the perfect tool for your health plan to immediately comply with the CMS Interoperability and Patient Access Final Rule as well as the 2020 Medicaid Managed Care Final Rule. Our healthcare provider directory, Convergent, bridges the gaps in fragmented, poor quality provider listings across institutions, systems of care and technology platforms. This data-as-a-service solution uses proprietary matching and cleansing algorithms to sift through and unify provider data from large public and proprietary data sets. The fully FHIR 4.0 compliant suite of APIs and mobile-friendly user interface provide health plans and Medicaid agencies with clean, curated and always up-to-date network data. Don’t wait, start working on directory compliance now that works as a sure investment in the future.
The Challenge: VillageCare’s numerous provider data operations were time-consuming to maintain and error-prone.
VillageCare received raw data extracts from their third-party administrator (TPA) that necessitated monthly master list updates through an unwieldy manual process to create and disseminate provider directories to their members. The process resulted in time delays and data inaccuracies that frustrated VillageCare and its members. There were data disconnects between the web search experience and which doctors were actually in network and at what locations.
Meanwhile, The CMS Interoperability and Patient Access Final Rule requires managed care plans to make a FHIR-compliant provider directory available to patients. New Managed-Care Organization (MCO) rules also require that the user interface (UI) for a provider directory be compliant with the Policy for Section 508 Compliance and Accessibility of Information and Communications Technology (ICT).
To solve for these multiple challenges and meet the new requirements, VillageCare needed a UI that would provide improved, 508-compliant accessibility and search parameter capabilities, and which could smoothly integrate with their new provider directory FHIR APIs.
The Solution: Leap Orbit’s modern provider search experience UI uses VillageCare’s FHIR 4.0.1 API
The mobile-responsive provider search solution integrates with VillageCare’s new FHIR server, enabling the combination of multiple FHIR resources (Practitioner, Practitioner Role, Organization, and Affiliations). Leap Orbit’s design is simple, with an accessibility-first approach. It is 508 compliant and adheres to current WCAG standards. To preserve VillageCare’s ability to comply with the requirement to furnish hard copies of the directories, Leap Orbit implemented access to their partner, Command Direct to the FHIR server to continue the printing and distribution of provider directories to members.
The Outcome: VillageCare’s provider search now always has its most current provider data, showcasing its network for all beneficiaries to access
This allowed VillageCare to eliminate additional steps it needed to update its previous search experience. All its data validation and update requirements now focus on producing their API which will be used for other similar use cases in the future. Leap Orbit’s search expereince also happens to be “white-labeleable” and customizable for any carrier’s FHIR API. Click here to try out VillageCare’s new provider search experience.
"…it was really great to find someone that was ready to go with this standard [FHIR] format" - Ku’uipo Curry, Director IT Data Management, VillageCare
Contact us here if you’d like to consolidate your provider data operations and create an improved member search experience.
About Leap Orbit
Founded in 2015, Leap Orbit is the trusted innovation partner to many of the market-leading health data networks, including CRISP, Manifest MedEx, and NEHII. Leap Orbit’s philosophy is to run toward healthcare’s biggest challenges, providing technology and solutions to assist with the opioid crisis and patient data privacy. Through its health organization partners, Leap Orbit’s work reaches at least 45 million patients from Alaska to Maryland. For more information, visit LeapOrbit.com and follow on LinkedIn.
About VillageCare
VillageCare is a community-based, not-for-profit organization serving people with chronic care needs, as well as seniors and individuals in need of continuing care and rehabilitation services.
Our mission is to promote healing, better health and well-being to the fullest extent possible. Our care is offered through a comprehensive array of community and residential programs, as well as managed care. VillageCare has provided health care services to individuals residing within New York City for over 40 years
by David Finney, Partner, Leap Orbit

In the first installment in this series, I made the case for modularity when it comes to a health plan’s provider data management strategy. I also preached from the gospel of strategic incrementalism. Sooner or later (usually sooner) during a health plan’s journey to the ultimate objective of an enterprise-wide provider data source of truth, we are asked to integrate with a critical, third-party system.
From its position as the source of truth, the Convergent Provider Data Hub can interact with these systems in a variety of ways. The third-party system can be a source of provider data for Convergent. Or the system can be a recipient or consumer of Convergent’s trusted data. In certain situations, a system maybe both. Here are a few real-world examples:
There are many ways to support system-to-system interoperability, and we’ve been thoughtful to build Convergent to support virtually all of them. But Restful APIs are quickly becoming the game-changer in healthcare that they are in other sectors. In particular, CMS’s full-throated endorsement of HL7’s FHIR standard, in the Interoperability Rule and elsewhere, is opening new frontiers for interoperability and automation for health plans. As FHIR becomes ubiquitous, the path to achieving the objective of an enterprise-wide source of truth for provider data will become even smoother.
Provider directories not only help members find health care, they are pivotal in achieving operational efficiency and meeting regulatory standards. Maintaining provider data management and up-to-date provider directories is essential for the success of health plans. Provider directory automation is an investment in the future of your health plan and your members. Here are five compelling reasons to transition from outdated, legacy processes to a streamlined, automated system:
Outdated or incorrect provider information often results in low rates of first-pass claims payments. Automating your provider data ensures accuracy, aligning submitted claims with current data, thus facilitating the claims process. This accuracy also mitigates issues in complaints and grievances processes, driving efficiency in these critical areas.
With the healthcare industry under scrutiny for wasteful spending, federal laws like the No Surprises Act are putting pressure on health plans to maintain current provider directories. Plans face new risks for the consequences of unexpected out-of-network charges, and the trajectory of this regulatory activity is clear: plans will be held accountable for failing to clean up provider networks.
The US is experiencing a mental health crisis inaccurate listings of health care providers who are not actually available for appointments (e.g.: not accepting new patients, retired, moved away, or no longer accepting the particular type of insurance)., often referred to as “ghost networks,” negatively impact member satisfaction. Ensuring accurate and accessible provider information is crucial, not just for member satisfaction but also for addressing broader public health challenges due to inadequate access to care.
Automating provider data operations streamlines the onboarding process. Plans that can incorporate reference data at scale and leverage modern technology no longer struggle manually with delegated rosters, sanctions checks and expirables. Whether credentialing in-house or leveraging a CVO, all plans have opportunities to make onboarding more seamless.
To build a business case for investing in provider data automation, look at your people. Automation can free up your team from the time-consuming task of manually reviewing, managing and manipulating provider records, allowing them to focus on more strategic initiatives. This shift not only saves time but also translates into significant cost savings for your organization. Your team will thank you for the shift away from spreadsheets, flat files, and Access databases.
See how VillageCare used Convergent to Automate Their PNDS Reporting Error.
In a detailed discussion with Julie Barnes, founder and CEO at Maverick Health Policy, we delve into the intricacies of the No Surprises Act and its implications for healthcare providers, insurers, and consumers. With her extensive background in healthcare policy and strategic advising, Julie provides valuable insights into how this legislation aims to transform healthcare cost management and enhance patient protection.
Please enter correct post id for Video SEO Post
Key topics covered in this interview include:
02:20 -- Overview of the No Surprises Act's Price Transparency Mandates
05:41 -- Advanced Explanation of Benefits (EOBs)
11:39 -- Impact on Health Plans and Insurance Providers
14:10 -- Impact on Premiums
18:43 -- Price Comparison Tool
22:02 -- API Economy
24:30 -- Data Liquidity
26:13 -- Provider Directories
32:45 -- The Critical Role of Health IT in Implementing New Policies
41:30 -- Challenges for Health Plans
44:46 -- The New Business Truth
50:40 -- Future Implications for Healthcare Costs and Consumer Protection
The No Surprises Act, which generally went into effect January 1, 2022, seeks to protect consumers from unexpected medical bills from out-of-network services. Julie Barnes explains the act's primary goals and the mechanisms it puts in place to ensure price transparency and reduce the financial burden on patients.
1. Understanding the No Surprises Act: Julie outlines the core components of the No Surprises Act, focusing on its intent to shield consumers from the shock of surprise medical bills. This legislation mandates that patients only pay in-network costs for out-of-network emergency services, fundamentally changing how patients are billed for unexpected care.
2. The Role of Advanced Explanation of Benefits (EOBs): One significant provision of the No Surprises Act is the requirement for providers to offer an advanced Explanation of Benefits. This document must outline the estimated charges for healthcare services before they are rendered, including whether a provider is in-network and the estimated cost the patient will bear. Julie discusses the operational challenges this poses for healthcare plans and the potential benefits for patient financial planning.
3. Impacts on Health Plans: The Act requires significant adjustments from health plans regarding network management and billing practices. Julie highlights how health plans need to enhance their data management systems to ensure compliance and prevent billing errors that could lead to penalties or patient dissatisfaction.
Julie emphasizes the importance of health information technology in implementing the No Surprises Act. Advanced data management systems are essential for maintaining up-to-date provider directories, accurate billing information, and compliance with the transparency requirements of the Act.
1. Enhancing Provider Data Management: Effective management of provider data is crucial for the accuracy of advanced EOBs and compliance with network adequacy requirements. Health IT systems must be capable of updating provider information in real-time to ensure that data reflects current network statuses.
2. Future Challenges and Opportunities: The integration of robust health IT solutions will be critical in addressing the challenges posed by the No Surprises Act. Julie suggests that future regulations will likely push for even greater data integration and interoperability among healthcare providers and insurers.
Julie Barnes' insights into the No Surprises Act provide a clear roadmap for healthcare providers and insurers preparing to navigate this new regulatory environment. With the right strategies and technologies, the healthcare industry can effectively implement these changes, leading to more transparent billing practices and enhanced patient protection.
Julie Barnes is a health care policy expert with years of experience helping the private sector navigate federal government activities that impact the health care system. Ms. Barnes is a strategic adviser to organizations that need guidance about federal health policies and how to develop relationships with policymakers and influential advocacy organizations.
As a former policy analyst, health care attorney, and Capitol Hill staffer, Ms. Barnes can inform business strategy and investments in a myriad of health care areas, including health information technology, data privacy and interoperability, value-based care, transparency, health insurance and new payment models, and federal health programs.
by Jake Tunney, Product Manager, Leap Orbit
Delegated roster submission can be a challenging process, creating friction between plans and providers, and frustrating members by creating delays in updates to your directory and claims system.
A lot of times it looks like this:
Even when using alternatives like CAQH Proview, plans need providers to register and be proficient in using CAQH. Meanwhile, recent numbers show less than 1/3 of healthcare providers in the United States use CAQH ProView (Source)
Now with Convergent's Delegated Roster Upload tool, you can do this all in one step:
The result is an improvement in roster intake speed by up to 96% and over 90% cost savings on manual processes.
Contact us here if you’d like to explore more!!!
by Jake Tunney, Product Manager, Leap Orbit
Rosters taking 45 days to upload? Changes you submitted last year, are still being “worked?” There are a number of problems providers face when trying to get their data updated on plans’ directories. Let’s try to find out. Where do these rosters go?

Well, we know they start on websites like this, asking for either ProView or an email submission with their roster template:
Only about one-third of provider groups use CAQH ProView for Groups, so many have to submit via email or SFTP. This is the first red flag that this is an outdated process.
If you read the fine print, this plan asks for an update every 90 days and to allow for at least 30 days for changes to be made on their side.
This is technically a No Surprises Act violation by the plan as all provider updates now need to be processed in 2 days.
Now let’s look behind the scenes at what a plan’s process looks like:

This is an actual health plan's roster submission process. If you’ll notice, after the data is taken in via SFTP (a seriously outdated technology) the data has to pass through 5 steps and 3 individuals’ custom processes before an error report is generated in Tableau and the process repeats itself. Once the roster is “clean,” then it is submitted to the claims system and directory. A number of things have to go right for provider data to be updated.
The crazy part about this is this happens to be a “good” process. This is a classic case of healthcare being at least a decade behind current technology best practices.
Between the overly complex process and a “user-unfriendly” experience for providers, it’s no surprise that providers are frustrated with these delegated credentialing processes.
That’s why I’m proposing introducing a new, modern approach that is consistent between industries. Introducing, Convergent’s Delegated Roster Upload Tool.
Your provider groups will love our simple delegated roster upload tool - and you will too!

We’re reducing data upload time by 96% while improving directory accuracy by up to 97%. And all while using simple, modern technology that’s been adopted a million times over by other industries. If you’d like to learn more, let’s hop on a call for a short demo by clicking here or click here to try it out.